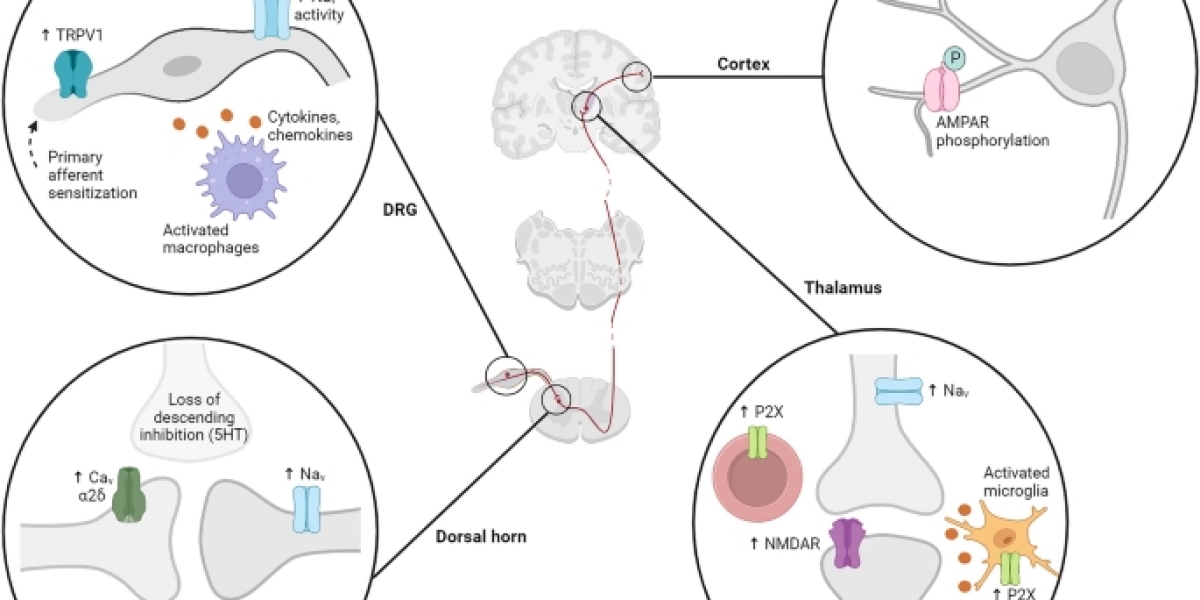
Central neuropathic pain (CNP) is a challenging and often debilitating form of chronic pain that arises from dysfunction or damage to the central nervous system (CNS). Unlike nociceptive pain, which stems from tissue damage or inflammation, central neuropathic pain results from aberrant processing of signals within the brain or spinal cord. In this exploration, we delve into the complexities of CNP, examining its causes, symptoms, diagnostic approaches, and potential treatment modalities.
Causes of Central Neuropathic Pain:
CNP is often associated with injuries or diseases that affect the CNS. Common causes include:
- Spinal Cord Injury: Traumatic injury to the spinal cord can disrupt normal nerve signaling, leading to persistent pain.
- Multiple Sclerosis (MS): In MS, an autoimmune condition, the protective covering of nerve fibers is damaged, causing miscommunication of signals and resulting in neuropathic pain.
- Stroke: A stroke can lead to damage in specific areas of the brain, triggering central neuropathic pain.
- Brain Trauma: Injuries to the brain, whether from trauma or surgery, can cause alterations in nerve function, leading to chronic pain.
- Infections of the CNS: Certain infections, such as meningitis or encephalitis, can damage CNS structures, contributing to neuropathic pain.
Symptoms of Central Neuropathic Pain:
The manifestations of CNP can vary widely, but common symptoms include:
- Burning Sensation: Individuals with CNP often report a persistent burning sensation, which can be localized or widespread.
- Electric Shock-like Pain: Sudden, sharp, and stabbing sensations resembling electric shocks are characteristic of CNP.
- Allodynia: Increased sensitivity to stimuli that are not typically painful, such as light touch or clothing brushing against the skin.
- Hyperalgesia: Exaggerated responses to painful stimuli, where even mild pressure can cause intense discomfort.
- Numbness or Tingling: Some individuals may experience numbness, tingling, or a loss of sensation in affected areas.
Diagnostic Approaches:
Diagnosing CNP requires a comprehensive evaluation by healthcare professionals, often involving neurologists or pain specialists. Key diagnostic approaches include:
- Medical History and Physical Examination: A thorough review of the patient's medical history and a detailed physical examination help identify potential causes and assess the nature of the pain.
- Imaging Studies: Magnetic Resonance Imaging (MRI) or Computerized Tomography (CT) scans may be used to visualize the CNS structures and detect abnormalities.
- Neurophysiological Tests: Electromyography (EMG) and nerve conduction studies can assess the functioning of peripheral nerves and identify abnormalities.
- Quantitative Sensory Testing: This involves assessing the patient's response to various sensory stimuli to evaluate the extent of sensory abnormalities.
Treatment Modalities for CNP:
Managing central neuropathic pain is challenging, and a multidisciplinary approach is often necessary. Treatment modalities may include:
Medications:
- Antidepressants: Tricyclic antidepressants (TCAs) and selective serotonin and norepinephrine reuptake inhibitors (SSNRIs) may help modulate pain signals.
- Anticonvulsants: Medication like pregabalin 75 mg capsules can be effective in dampening abnormal nerve firing.
- Opioids: In some cases, opioid medications may be prescribed for pain relief, although their use is often carefully monitored due to the risk of dependence.
Physical Therapy:
- Physical therapy aims to improve mobility, reduce muscle stiffness, and alleviate pain through targeted exercises and interventions.
Nerve Blocks and Injections:
- Local anesthetic or corticosteroid injections may be administered to block pain signals in specific nerve pathways.
Neuromodulation Techniques:
- Spinal cord stimulation and deep brain stimulation are emerging as potential options for managing CNP by modulating neural activity.
Challenges and Future Directions:
CNP poses significant challenges for both patients and healthcare providers. Its chronic nature, complex etiology, and variable response to treatments make it a condition that often requires ongoing management. Research into novel therapies, including targeted drug development and advanced neuromodulation techniques, offers hope for more effective and personalized approaches to CNP.
Holistic Care and Patient Support:
Living with central neuropathic pain can have profound effects on an individual's quality of life. Holistic approaches, such as mindfulness practices, stress reduction techniques, and support groups, play a crucial role in addressing the emotional and psychological impact of CNP. Comprehensive care extends beyond pharmacological interventions to encompass the broader aspects of well-being.
Conclusion:
Central neuropathic pain, arising from disruptions in the central nervous system, represents a complex challenge in the realm of chronic pain management. Understanding its causes, recognizing diverse symptoms, and employing a multifaceted treatment approach are essential for improving the lives of individuals grappling with this intricate condition. As research progresses and medical interventions evolve, there is optimism for enhanced therapeutic strategies that can offer relief and improve the overall well-being of those affected by central neuropathic pain.