Male infertility stands as a formidable and often underestimated challenge within the realm of reproductive health, impacting millions of couples globally. While historical emphasis has centered around fertility issues in women, the significance of comprehending male infertility cannot be emphasized enough. This article aims to explore the diverse dimensions of male infertility, encompassing its origins, diagnostic approaches, and potential avenues for treatment, spotlighting a critical subject in the realm of reproductive health.
Causes of Male Infertility:
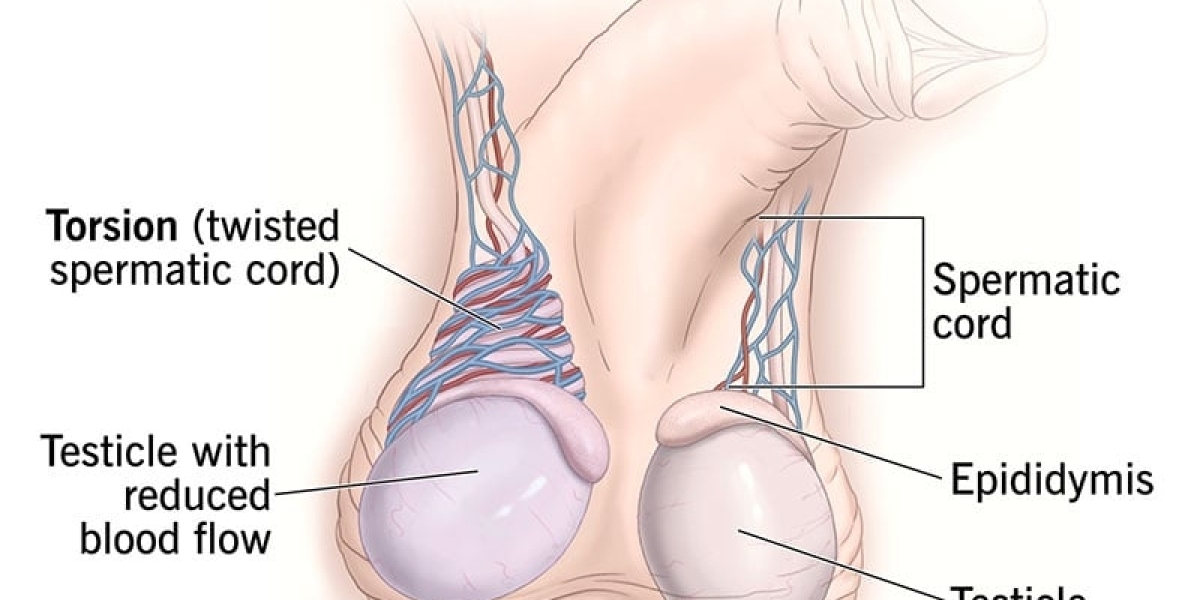
Male infertility is a result of an intricate interplay of various factors, involving both physiological and lifestyle-related components. A key contributor lies in abnormal sperm production or function. Conditions such as varicocele, hormonal imbalances, genetic factors, and infections can exert adverse effects on sperm production and quality. Lifestyle choices, including smoking, excessive alcohol consumption, drug abuse, and obesity, also wield a substantial influence on male fertility.
Diagnosis of Male Infertility:
Accurate diagnosis serves as the foundational step in addressing male infertility. Healthcare professionals utilize an array of tests and evaluations to pinpoint underlying causes. Semen analysis, a fundamental diagnostic tool, scrutinizes sperm count, motility, and morphology. Hormonal tests reveal imbalances that may impact fertility, while imaging studies, such as ultrasound, can detect structural abnormalities like varicoceles.
In some instances, genetic testing may be recommended to ascertain if hereditary factors contribute to male infertility. Comprehensive testing empowers healthcare providers to tailor treatment plans to the specific needs of individuals or couples.
Treatment Options:
The treatment of male infertility hinges on identified causes and spans from lifestyle adjustments to medical interventions. Lifestyle modifications, such as regular exercise, a balanced diet, and avoiding harmful substances, can significantly enhance fertility.
To address hormonal imbalances, one might contemplate the exploration of hormone replacement therapy. Effectively repairing varicoceles through surgical interventions, like varicocelectomy, stands as another avenue to restore fertility. In instances where genetic factors come into play, viable solutions may manifest through the adoption of assisted reproductive technologies (ART), including procedures like in vitro fertilization (IVF) coupled with intracytoplasmic sperm injection (ICSI).
Addressing the Emotional Aspect:
Coping with infertility can exact a toll on the emotional well-being of individuals and couples. Recognizing the psychological impact is essential, urging individuals to seek support when needed. Counseling, participation in support groups, and fostering open communication between partners play pivotal roles in navigating the emotional challenges linked to male infertility.
Hope on the Horizon:
Advancements in reproductive medicine instill hope for couples grappling with male infertility. Ongoing research explores innovative treatments, including stem cell therapy and gene editing techniques, holding the potential to revolutionize the field. As our understanding of male infertility deepens, the spectrum of available interventions broadens, fostering optimism for those facing challenges in conceiving.
Male infertility, a complex and multifaceted issue, necessitates a comprehensive approach encompassing diagnosis, treatment, and support. Elevating awareness and understanding of male reproductive health empowers individuals and couples to seek timely intervention, dismantling the stigma surrounding fertility issues. Through a blend of medical advancements, lifestyle adjustments, and emotional support, the journey to overcoming male infertility becomes more manageable, renewing hope for those aspiring to build or expand their families.