How Diabetes Affects the Eyes
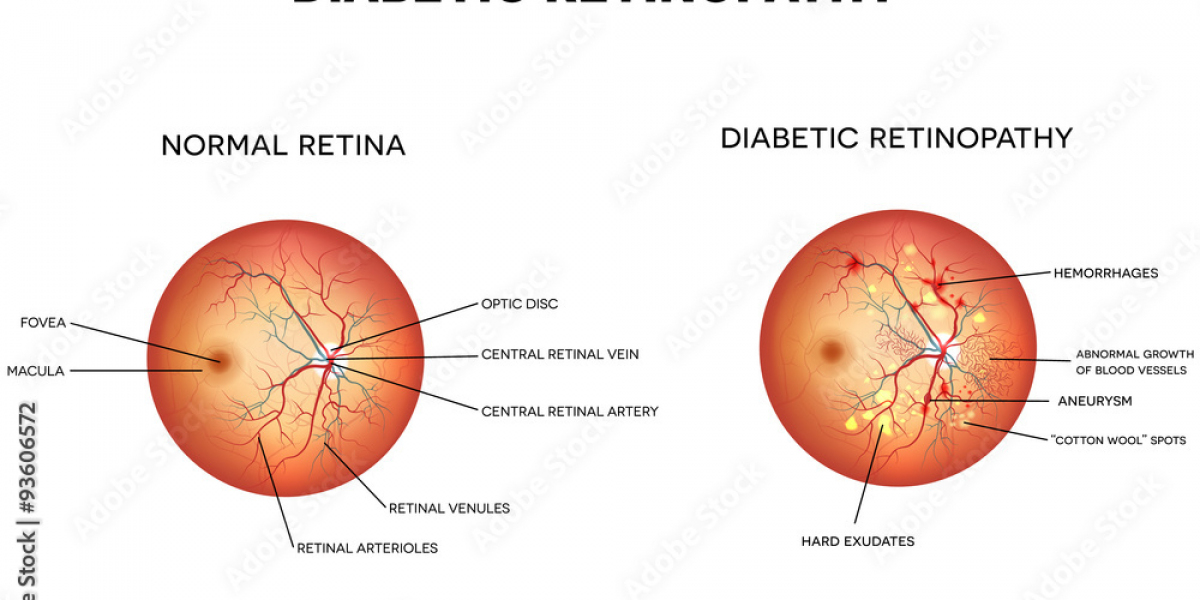
High blood sugar levels associated with diabetes can damage the blood vessels throughout your body, including those in your eyes. Over time, this can cause the small blood vessels in the retina to weaken, leak fluid, or even bleed. These changes can block light from reaching the retina and, if severe, may result in vision problems.
Diabetic retinopathy typically develops over time and affects people with both Type 1 and Type 2 diabetes. The longer you’ve had diabetes and the less controlled your blood sugar levels are, the higher your risk of developing this condition. High blood pressure and high cholesterol can also contribute to the progression of diabetic retinopathy.
The Stages of Diabetic Retinopathy
Diabetic retinopathy progresses through several stages:
Mild Non-Proliferative Retinopathy: In the earliest stage, small areas of the blood vessels in the retina weaken and form tiny bulges called microaneurysms. These bulges may leak fluid into the retina, causing mild vision disturbances.
Moderate Non-Proliferative Retinopathy: As the disease progresses, the blood vessels become more damaged, and their ability to transport blood to the retina is impaired. This can lead to retinal swelling and further vision impairment.
Severe Non-Proliferative Retinopathy: At this stage, a significant portion of the retinal blood vessels is blocked, depriving areas of the retina of oxygen and nutrients. The retina may signal the body to grow new, abnormal blood vessels as a response.
Proliferative Diabetic Retinopathy: This advanced stage is characterized by the growth of abnormal, fragile blood vessels in the retina. These vessels can bleed into the vitreous (the clear, gel-like substance in the eye), leading to severe vision problems. Scar tissue may also form, potentially causing retinal detachment, a condition that requires immediate treatment to prevent blindness.
Symptoms of Diabetic Retinopathy
In the early stages, diabetic retinopathy may not cause any noticeable symptoms. However, as the condition progresses, you may begin to experience:
- Blurred vision
- Difficulty seeing at night
- Dark spots or floaters in your vision
- Sudden vision loss
If you notice any of these symptoms, it’s important to schedule an eye exam immediately. Early detection can prevent further damage and help preserve your vision.
Preventing and Managing Diabetic Retinopathy
The key to preventing and managing diabetic retinopathy is maintaining good control over your blood sugar, blood pressure, and cholesterol levels. Regular eye exams are also essential, especially if you’ve been diagnosed with diabetes. The earlier diabetic retinopathy is detected, the more effective treatment can be.
Here are a few important steps to protect your vision if you have diabetes:
- Keep Blood Sugar Under Control: Properly managing your diabetes through diet, exercise, and medication can help slow the progression of diabetic retinopathy.
- Monitor Blood Pressure and Cholesterol: Keeping these within healthy ranges will reduce the strain on your eyes and other organs.
- Quit Smoking: Smoking can worsen diabetic complications, including those affecting the eyes.
- Regular Eye Exams: Annual comprehensive eye exams with dilation are crucial for detecting diabetic retinopathy early.
Treatment Options for Diabetic Retinopathy
If diabetic retinopathy is detected, there are several treatment options available, depending on the stage and severity of the condition. These include:
Laser Therapy (Photocoagulation): Laser treatment can seal leaking blood vessels and prevent new ones from forming, helping to control the progression of the disease.
Anti-VEGF Injections: Medications such as anti-vascular endothelial growth factor (VEGF) injections can help reduce swelling in the retina and inhibit the growth of abnormal blood vessels.
Vitrectomy: In advanced cases of proliferative diabetic retinopathy, a vitrectomy may be needed. This surgical procedure removes blood from the vitreous and scar tissue from the retina, improving vision and preventing further damage.
Your Kannur eye specialist will work with you to create a personalized treatment plan based on the stage of your diabetic retinopathy and your overall health.
Conclusion: Early Detection is Key
Diabetic retinopathy is a serious eye condition that can lead to vision loss if not properly managed. However, with regular eye exams, good diabetes control, and timely treatment, the progression of this disease can be slowed or even stopped. If you have diabetes, don’t wait until symptoms appear—schedule a comprehensive eye exam with a trusted Kannur eye specialist to protect your vision and maintain your eye health for years to come.