First of all,
The complex neurodevelopmental disorder known as attention deficit hyperactivity disorder (ADHD) has a significant influence on people in many aspects of their lives. In order to fully understand ADHD, a comprehensive investigation is necessary. This will entail examining the disorder's various presentations, possible causes, intricate diagnostic procedures, neurological underpinnings, environmental factors, pervasive effects on day-to-day functioning, treatment modalities, and subtle factors to take into account as a person develops.
Comprehending the ADHD Spectrum:
ADHD is a disorder that is difficult to classify into discrete subtypes, including inattentive, hyperactive-impulsive, and mixed presentations. ADHD that is mostly hyperactive-impulsive presents as restlessness and impulsivity, whereas ADHD that is predominantly inattentive shows difficulties focusing and organizing tasks. Both aspects are interwoven in the combined presentation, which highlights the need for a nuanced understanding that is specific to each person's experience.
Difficulties with Diagnosis:
Making the diagnosis of ADHD is a complex process that entails a thorough assessment that includes observations, interviews, and standardized questionnaires. Despite these techniques, problems like underdiagnosis and misdiagnosis continue because of social assumptions and symptom overlap with other mental health issues. It is imperative to tackle these diagnostic obstacles in order to ensure precise identification and prompt intervention, so establishing the groundwork for a more knowledgeable and compassionate approach.
The Neurobiology of ADHD:
The complex neurobiological foundations of ADHD have been revealed by recent developments in neuroscientific research. It has been determined that attention, impulse control, and executive skills are correlated with certain brain regions that exhibit structural and functional problems. ADHD symptoms are largely caused by dysregulation of neurotransmitters, especially norepinephrine and dopamine. Gaining an understanding of these subtleties of neurobiology is crucial to creating focused interventions that target the underlying causes of the illness and offer more potent forms of treatment.
Environmental and Genetic Influences:
A complex interaction between genetic predisposition and environmental factors leads to the development of ADHD. Environmental factors such prenatal exposure to tobacco smoking, premature birth, and low birth weight have been linked to an increased risk of developing ADHD, even if a major genetic component is still clearly present. The risk is increased when environmental pollutants such as lead are exposed early in life. For a thorough understanding of ADHD and the creation of successful treatment plans, it is critical to acknowledge the interaction of hereditary and environmental components.
The Effect on Everyday Life:
The effects of ADHD go beyond diagnostic standards and affect many aspects of day-to-day living. ADHD sufferers frequently struggle with emotional instability, poor social interactions, and difficulties in their academic and professional lives. Feelings of irritation, low self-esteem, and worry are among the consequences of ongoing difficulties with organization, time management, and task completion. Managing the rigors of everyday living necessitates a comprehensive and customized strategy that takes into account the range of experiences within the ADHD spectrum and tackles both the primary symptoms and the correlated deficits.
Treatment Strategies:
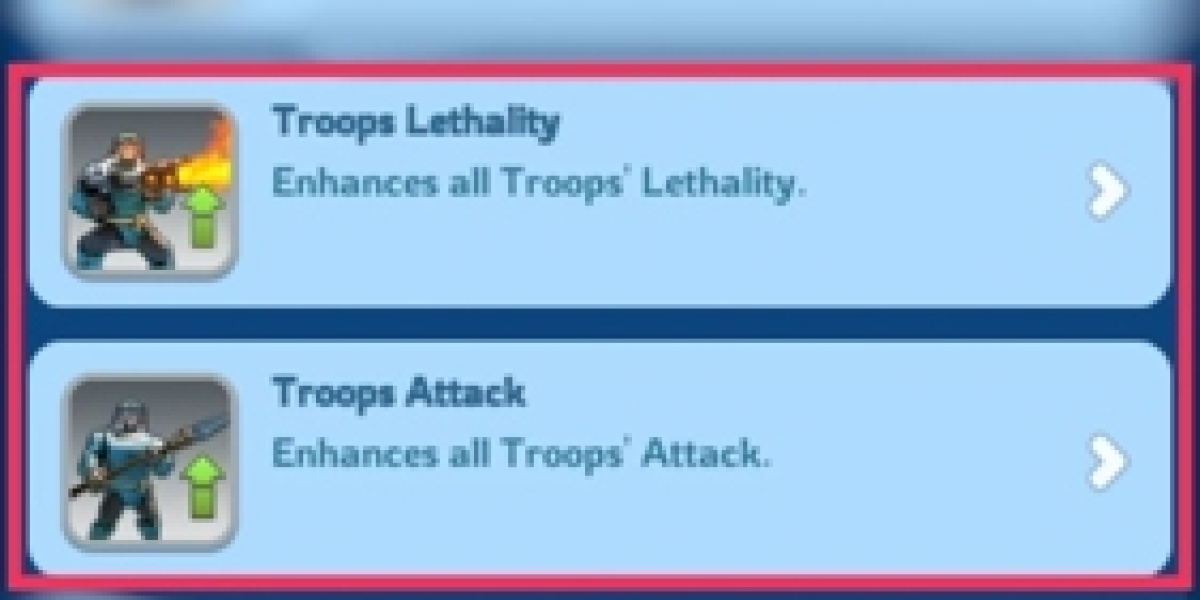
Behavioral therapies, psychoeducation, and, in certain situations, medication are all necessary components of a multimodal strategy for managing ADHD. Behavioral therapies concentrate on developing skills, organizing techniques, and flexible coping strategies to enable people to effectively handle obstacles in their daily lives. Psychoeducation is essential for improving understanding for people with ADHD and their families, as well as for creating a supportive and empathetic atmosphere. Certain symptoms can be treated and cognitive performance improved with the prescription of medications, including both stimulants and non-stimulants. Medication decisions should be made collaboratively, taking into account each patient's needs as well as possible side effects and long-term consequences.
Lifespan Considerations:
The effects of ADHD persist throughout adolescence and adulthood; it is not a static condition limited to childhood. As they get older, some people might notice a decrease in their symptoms, but others might still have major difficulties. Understanding that ADHD is a lifelong condition highlights the value of individualized treatments, continuous support, and a sophisticated grasp of the disorder's various developmental phases.
ADHD in adolescence:
For those with ADHD, the shift from childhood to adolescent brings with it a new set of difficulties. The temptation to live up to social norms increases, academic demands get more complex, and social dynamics get more intense. Teens with ADHD may struggle with problems like poor academic performance, damaged relationships with family and friends, and a higher likelihood of acting impulsively. In order to minimize potential long-term effects and enable adolescents with ADHD to successfully traverse the challenges of adolescence, early intervention and support are essential throughout this age.
ADHD in Adulthood:
Despite what many have historically believed, ADHD does not go away as an adult. Many people still struggle with issues of impulsivity, executive functioning, and attention. Adult ADHD symptoms can vary, with sufferers experiencing challenges with organizing their life, managing their time, and maintaining focus on tasks. The effects on relationships with others, work performance, and general quality of life require a customized approach to diagnosis and treatment. Acknowledging adult-onset ADHD allows people to get the help and resources they need, which improves their ability to adapt and succeed in different areas of their lives.
Coping Mechanisms and Support:
Using coping mechanisms and creating a supportive atmosphere are beneficial for people with ADHD at any stage of their lives. Behavioral techniques, such as psychoeducation and cognitive-behavioral therapy, give people the tools they need to better organize their lives, control their symptoms, and exercise self-control. Using assistive technologies, dividing work into managing chunks, and establishing disciplined routines are useful tactics that can greatly reduce the difficulties brought on by ADHD. Social support from friends and family is essential for building resilience and enhancing one's capacity to deal with the challenges of everyday life.
Educational Interventions:
Understanding and addressing the various learning styles linked to ADHD is crucial in the field of education. An inclusive learning environment can be established through individualized education plans (IEPs), differentiated instruction, and access to support resources. Teachers are essential in helping kids develop empathy and understanding by using tactics that are specifically designed to meet the requirements of students with ADHD. Improved academic results and the development of critical life skills are facilitated by early identification and intervention in the educational context.
Employment Considerations:
The effects of ADHD continue throughout adulthood and have an impact on career paths and vocational performance. It can be difficult for people with ADHD to stay focused, fulfill deadlines, and efficiently manage their time. Task delegation, open communication, and flexible scheduling are examples of workplace adjustments that can improve output and job satisfaction. Educating coworkers and employers about ADHD promotes a diverse and encouraging work environment.
Beyond Drugs: Comprehensive Methods for Managing ADHD:
Although drugs are an important part of treating ADHD symptoms, comprehensive methods that emphasize general wellbeing are becoming more and more popular. A balanced diet, adequate sleep, and regular exercise are examples of lifestyle changes that might enhance general health and potentially lessen the symptoms of ADHD. Meditation and yoga are two examples of stress-reduction mindfulness and practices that have demonstrated potential in improving focus and reducing impulsivity. By combining these all-encompassing methods with established therapies, people can manage their ADHD and improve their quality of life with a complete toolkit.